90834
By Kimberly J. Soenen | January 27, 2025
Dear Readers,
Today, THE FINE PRINT Health Humanities Magazine launches its 2025 Winter/Spring editorial season.
Another season has begun, as well. Project 2025 is now being forcefully implemented by the current U.S. administration.
We remain committed to long-form writing, in-depth reporting, authorship, evidence-based fact checking, vetted data, high caliber visual journalism and original art.
People from diverse backgrounds, abilities, ages, crafts, trades, professions and academic disciplines will continue sharing their views on health, healthcare and Public Health in the name of betterment.
We will highlight exceptional exhibitions, reportage, films, documentaries, music, books and conversations ongoing that stand out as both constructive and solutions-oriented. And UpCode, our network of investigative journalists working to expose Harm-for-Profit and White-Collar Healthcare Crime will also continue its impactful collaborative work.
This week, we turn to the health of our Mental Health professionals.
Thank you for your reading and for your support~
Kimberly J. Soenen
Managing Editor, THE FINE PRINT Health Humanities Magazine
Founder and Executive Director, “SOME PEOPLE”
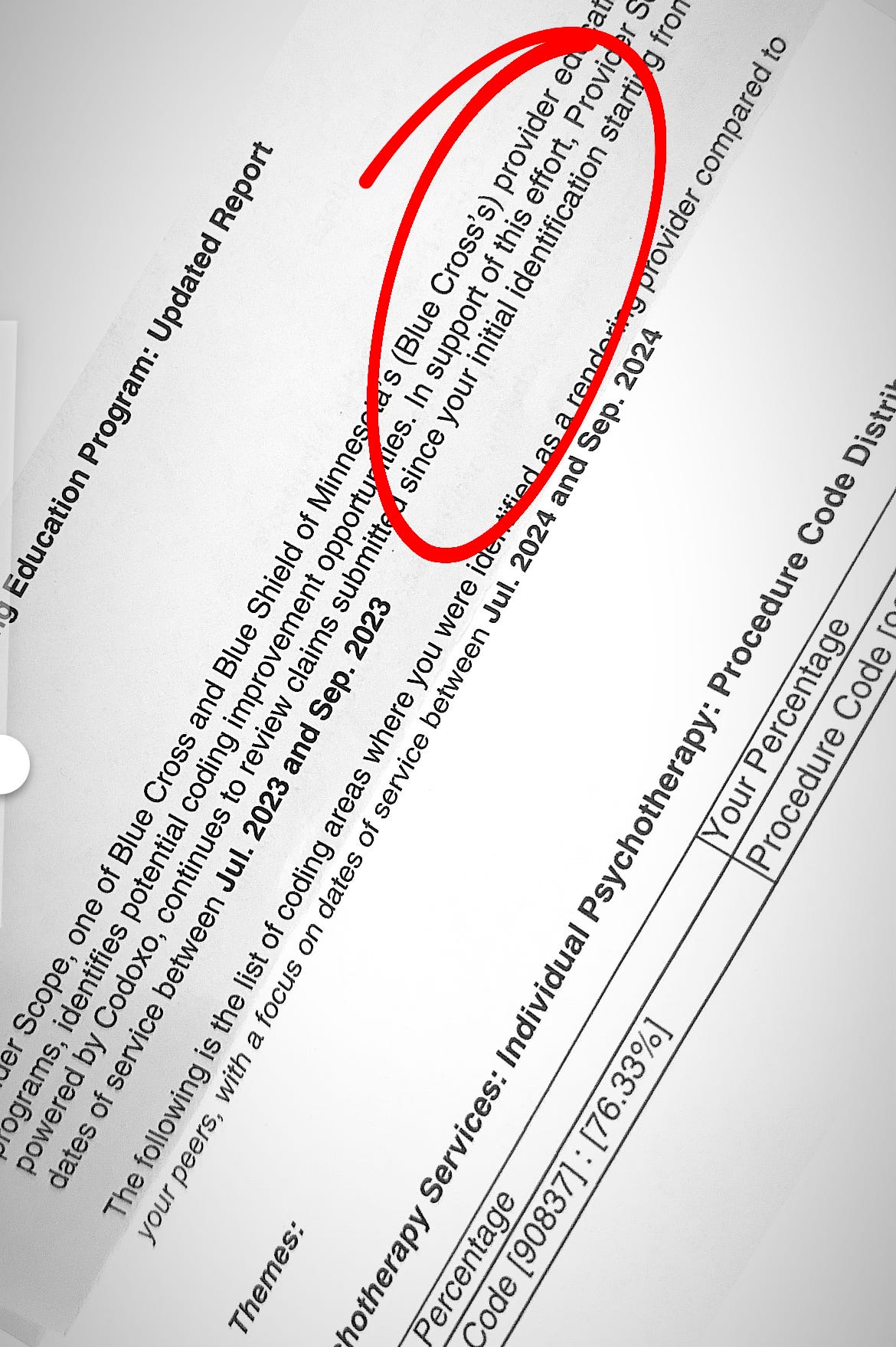
Americans may not be aware when they enter a Mental Health therapist’s office or log onto an online therapy session that the average session in the United States is limited to 53-60 minutes and is coded by Commercial Health Insurance companies as “90837.” This is called a Current Procedural Terminology (CPT) code by the industry.
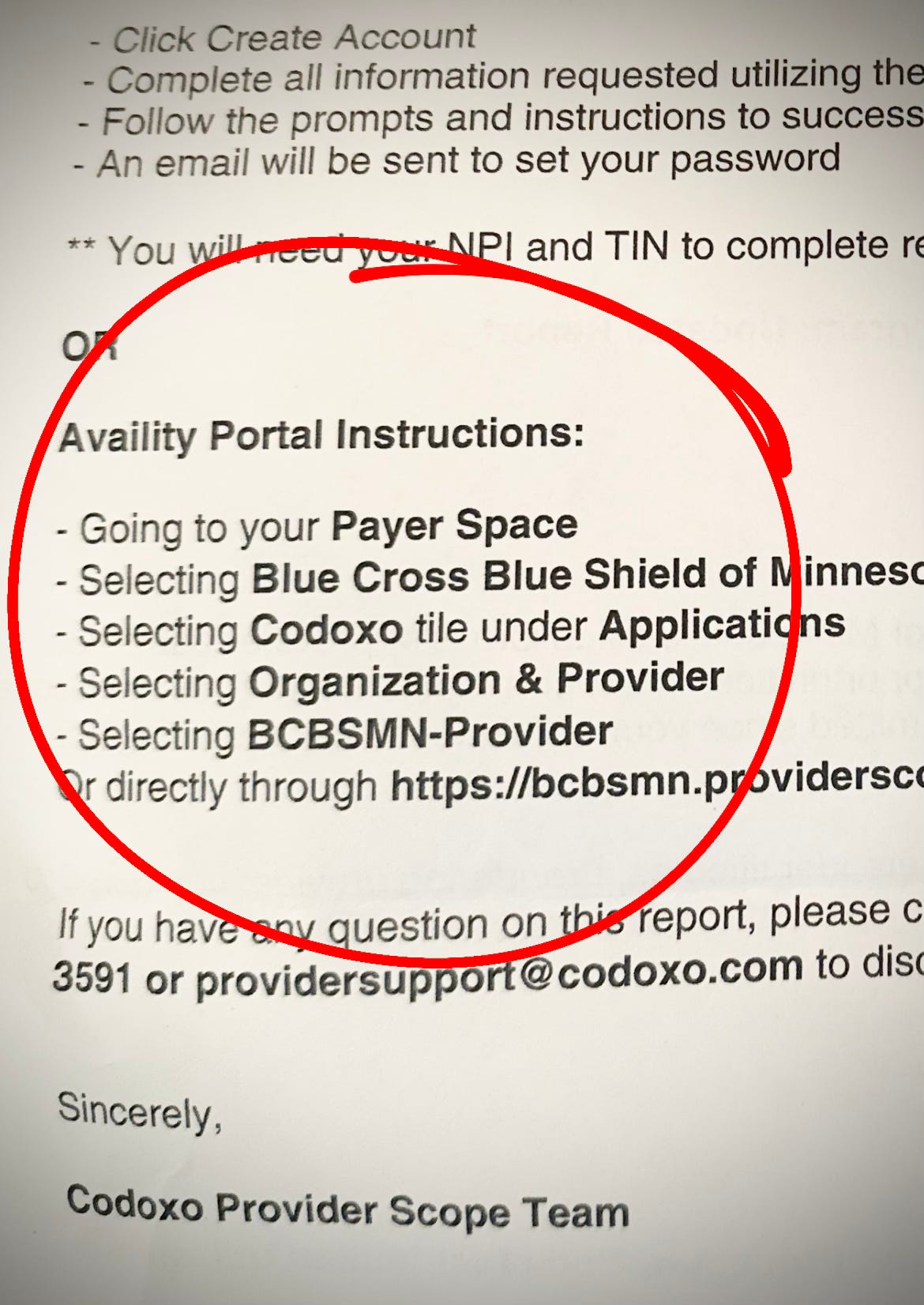
But there’s also code “90834,” a 38–45-minute session. Code 90834 pays providers less. Frequently, Commercial Health Insurance industry companies audit and threaten Mental Health therapists when we they use code 90837. These communiqués delay payment and are known as “Coding Improvement Opportunities.” Many Commercial Health Insurance industry companies have been called out and sued for the pressure, intimidation and harassment.
Like all ethical medical professionals, Mental Healthcare professionals are wedged between the Commercial Health Insurance industry and their patients. On one hand, Americans are hearing prescriptive PSA campaigns from the former United States Surgeon General and advocacy groups encouraging people to “seek out care,” but the reality is Commercial Health Insurance companies make it extremely difficult to access and afford consistent quality care.
I’ve been speaking with hundreds of Mental Healthcare professionals over the last four years about their day-to-day struggles and how they navigate the onerous administrative side of their job while trying to advocate for their patients. Jessica Ellison, M.A., L.P.C.C., is one. She has more than ten years of experience working with children and adolescents in academic, non-academic and clinical settings. She graduated from Hamline University and obtained her master’s degrees from St. Mary’s University. Her clinical experience includes working with children in their homes, foster homes, shelters and schools. She has been managing her own practice, J. Ellison and Associates, for eight years in Burnsville, Minnesota.
We have shared several phone conversations and email exchanges over the last three months. I began with a very basic question about this very high-stress profession and the responsibility of holding human lives in the balance.
Soenen: Why did you become a therapist?
Ellison: For those who know me, the most obvious reason I became a therapist would likely be that my father was one. As a child, I admired how he helped children and families, and I found it fascinating that he got to engage with toys as part of his work.
Initially, I pursued a degree in Neuropsychology with the intention of delving into research. However, I quickly discovered the highly political nature of academia, which led me to pivot toward psychology and counseling with the goal of creating my own practice—free from the constraints of working for someone else and their agenda.
Soenen: What it the most rewarding element of your work?
Ellison: I've always been deeply intrigued by human behavior: What defines me as an individual? How are we, as humans, so uniquely different, yet fundamentally similar in so many ways? I believe that many therapists are drawn to the field not only to help others but also to understand themselves and their place in the world. For me, being a therapist is an honor and a privilege—it's an opportunity to accompany my clients on their journey of healing, growth, and self-discovery.
Soenen: What is the most frustrating aspect of the United States Commercial Health Insurance industry for Mental Health providers?
Ellison: The most frustrating and anger-inducing aspect of the current healthcare system is the clear prioritization of profit over people. The healthcare model, especially within commercial health insurance, is designed to work against both patients and providers.
For patients, the barriers to receiving necessary care—whether it's due to financial constraints, insurance denials, or overwhelming premiums—are profoundly harmful. As a practitioner, it's heartbreaking to see clients struggle not just with their Mental Health, but also with accessing and affording the treatment they need. It’s demoralizing to witness people being priced out of healthcare, despite having health insurance that’s supposed to protect them.
Soenen: Is there discussion in your professional circles now about Moral Injury and the toll the Denial of Care business model takes on Mental Healthcare professionals?
Ellison: The emotional and physical toll on healthcare providers is significant. We are constantly navigating a system that is designed to complicate our ability to help others. The paperwork, the endless calls to commercial health insurance companies, the never-ending cycle of claim denials, the lack of respect for our expertise—all of this makes it harder to maintain the passion and energy needed to give patients the care they deserve. And all of this work, the emotional burden, and the stress are ultimately met with inadequate reimbursement, if anything at all.
As a provider, I feel personally impacted not just by the difficulties my patients face, but by the systemic failures that directly affect my ability to make a living doing what I love. This constant struggle with commercial health insurance companies, who are not accountable for their actions, leaves both the patients and the providers stuck in a cycle of stress, uncertainty, and burnout. The fact that profit-driven motives are allowed to dictate who receives care and at what cost undermines the very ethics of our profession, and as a result, both patients and practitioners suffer.
For healthcare professionals, the stress from these barriers is cumulative. We’re fighting for our clients, but at the same time, we're fighting to stay afloat ourselves—balancing financial survival with our commitment to healing. The physical and emotional toll of this is far-reaching and something people outside of the healthcare field often don't fully grasp.
Soenen: What Commercial Health Insurance industry business tactics have you experienced in recent years that impose distress to your practice, patients and business?
Ellison: As I enter my eighth year of private practice, I've noticed a pattern of tactics used, not only by UnitedHealthcare (UHC), but also by other Commercial Health Insurance industry companies.
At the beginning of the year, commercial health insurance companies are extremely slow to pay providers' claims. There are several reasons for this: clients have deductibles to meet and commercial health insurance companies change member numbers, group numbers, or payor IDs, which causes delays because providers have to resubmit claims weeks after the original submission.
Additionally, Commercial Health Insurance industry companies often change requirements for taxonomy codes and rendering provider IDs without informing providers ahead of time, further delaying payments.
Claims submitted at the end of the year and during January tend not to be paid until late February or March. Typically, contracts allow providers 60-90 days to submit claims for remittance. If providers do not submit before their grace period, they are not paid. However, Commercial health Insurance companies are required to process and pay providers within 30 days of receiving claims. When this contractual agreement is not met by the Commercial Health Insurance company, there are little to no consequences for the delay.
Soenen: Can you discuss how UnitedHealthcare intentionally delays payments?
Ellison: Last year, I was unable to get a clear answer from OPTUM Behavioral Health, which UHC uses to process Mental Health and Behavioral Health claims, regarding the interest owed for each day they did not process and pay the claims. The cybersecurity breach last spring made the delayed-payment period even longer. During this time, OPTUM initiated an investigation regarding claims from over two years ago, claiming I owed a large sum of money and would begin recouping it directly from my payments.
The situation involved a client with both primary and secondary insurance, one of which was UnitedHealthcare (UHC), and both used OPTUM Behavioral Health to process their claims. There was confusion over which insurance was primary and which was secondary, leading to numerous phone calls with insurance representatives, all of whom provided inconsistent answers.
Soenen: How did they help you?
Ellison: Ultimately, information that had been available to the insurance companies two years prior became my responsibility to resolve. After significant back-and-forth, the investigator handling my case decided to close it due to the insurance companies' lack of cooperation and transparency.
Despite following advice from an OPTUM Provider Advocate, I never received the remittance owed by the secondary insurance. This situation caused significant distress for me professionally and personally, as well as for my client, who was caught in the middle of these administrative errors.
Soenen: The weaponization of administrative chaos.
Ellison: Yes. Over the years UHC and other Commercial Health Insurance companies tell providers they’re receiving an increase for payments, however, the cost is being passed down to the member instead of the insurance company. This is deceptive and can be challenging for some clients’ financial situation.
“There are cases where patients cannot receive treatments because the commercial health insurance company won’t cover enough of the cost, making it unaffordable for the member. This kind of denial of necessary care is not only financially harmful to individuals but can lead to long-term health complications, further burdening the system and, ultimately, society.”
-Jessica Ellison, M.A., L.P.C.C.
Soenen: Your practice is currently “in-network” with Beacon/Value Options, Behavioral Health Systems, OPTUM, UMR, UBH, Medica, Medicaid (Medical Assistance), PreferredOne, UnitedHealthcare, Aetna, UCare, and Tricare but you are not ‘in-network” with Health Partners, Blue Cross Blue Shield, and Cigna. Cigna, UnitedHealthcare and Aetna are mired in White Collar Healthcare Crimes ongoing. What is the aspect of this lack of choice and crime that impacts you most as a therapist?
Ellison: What stands out most is the disparity in how healthcare operates. Commercial Health Insurance companies like UnitedHealthcare, should not be allowed to prioritize profit over people’s health. The very concept of a for-profit healthcare system is flawed when it comes to serving the public good. It’s important to remember that the passive harm caused by these companies is as violent as any other form of systemic oppression—it is covert, but it deeply affects people’s lives, creating a cycle of financial hardship and poor health outcomes that only deepen the divide between the haves and have-nots.
Soenen: How does the Commercial Health Insurance industry impact therapists in training?
Ellison: Post-graduate work for therapists typically requires 4,000 hours under the supervision of a licensed and board-approved supervisor within the requirements of their licensing board (e.g., the BBHT Board of Behavioral Health and Therapy). However, providers are not allowed to file claims with Commercial Health Insurance companies until they are fully licensed by their board. This includes face-to-face time with clients. Often, pre-licensed providers work in roles like ARMHS (Adult Rehabilitative Mental Health Services) and CTSS (Children’s Therapeutic Services and Supports), where they provide in-home and school-based services focused on skills, therapy, and counseling.
Without the ability to file claims under their supervisor’s license and NPI (National Provider Identifier), pre-licensed therapists have limited opportunities for training. This severely restricts their ability to gain the experience necessary for licensure, which could ultimately impact the availability of these services in the community Without these training options, there could be a greater strain on state and county social support systems, as fewer trained professionals would be available to provide these critical services. Pre-licensed therapists also gain experience by working in practice settings where they are supervised and can work directly with clients in therapy. This makes it difficult to train.
Soenen: With this barrier, how do post-graduate and pre-licensed therapists learn from mature and experienced veteran therapists?
Ellison: Without the ability to submit claims under a supervisor’s license and NPI, these training opportunities become financially unfeasible. This situation could leave post-graduate, pre-licensed therapists without any viable, paid options to gain the necessary experience and training.
Soenen: Is there a good faith back-channel work around to hurdle this barrier to training?
Ellison: Volunteering at community counseling centers is an alternative, but this often requires the supervisee to pay for supervision out-of-pocket while receiving no compensation for their work with clients. If UnitedHealthcare and other Commercial Health Insurance inudstry companies remove the ability for supervisors to bill for trainee and pre-licensed services, the path from post-graduate training to full licensure will effectively break down, resulting in fewer professionals entering the workforce and fewer services available to the community.
Soenen: What other tactics have you experienced by UnitedHealthcare over time that prevents you from performing your job optimally?
Ellison: Just the other day, I had to call to inquire about claims that were adjudicated but not paid. It turned out the issue was on UHC’s end—someone or something had failed to mark me as a provider who accepts state plans/medical assistance. This was a first in eight years of practice. When I asked if I’d be compensated for the delay in payment, especially since it was due to their error and the payment had passed the 30-day window, I knew the answer would be no.
This is a prime example of how UHC, along with other Commercial Health Insurance companies, makes it nearly impossible for small group and private practices to have any sense of security.
The administrative process is unnecessarily complicated, with inconsistent expectations and responses. They promise to call you back but rarely do. As a solo practitioner, I’ve spent countless hours on the phone with Commercial Health Insurance companies trying to follow up on unpaid claims, correct their errors, and hold them accountable to the contract we agreed upon.
Soenen: How do you navigate the distress UnitedHealthcare and others impose?
Ellison: More often than not, I don’t receive the compensation owed, any transparency, or any acknowledgment of responsibility on their end. They delayed payments at the beginning of the year for a reason, they deny responsibility for their failures and mistakes, and all of this leaves providers feeling defeated—while we're still expected to support our clients.
Soenen: How does the Denial of Care Harm-for-Profit business model effect you, not professionally, but personally.
Ellison: I’ll break it down for you. On the financial side, delayed payments made it difficult to maintain a consistent flow of income to support both my business and my family. With no clear answers as to when payments would be received or whether claims were accepted, I felt constant anxiety as a business owner. This uncertainty impacted my cash flow and made it challenging to confidently cover payroll and taxes due at the end of the first quarter.
Emotionally and physically, the one situation example I cited was extremely distressing, especially during the beginning of the year when Commercial Health Insurance industry companies are already notoriously slow to process claims.
The cyberattack in 2024 only amplified the stress, anxiety, and labor required to follow up on these claims and verify proper payment. The additional administrative burden took away valuable time and energy that I could have spent on my clients or personal well-being. This experience heightened my frustration and eroded trust in UnitedHealthcare and other Commercial Insurance industry companies, particularly their commitment to supporting providers and members alike.
As far as the impact on my patients, many patients, especially those aware of the cyberattack, were confused and anxious about the possibility of their personal information being leaked. As a provider, I felt it was crucial to inform clients about the situation so they could make informed decisions about their healthcare. Despite the gap in pay, I continued to see clients, driven by the principle of Do No Harm that is fundamental to all healthcare professions. This commitment underscored my responsibility to prioritize patients' needs, even under significant strain.
Soenen: How do you manage and why do you keep going?
Ellison: UnitedHealthcare and other Commercial Health Insurance industry companies present several challenges for providers, hindering our ability to deliver optimal care. One of the most significant obstacles is the ongoing pressure to adhere to their ever-changing requirements, which often seem to prioritize their bottom line over patient care. For example, UHC has made it difficult for providers to maintain accurate billing and payment systems, sometimes resulting in delayed or incorrect payments.
Soenen: Chaos and cost-shifting.
Ellison: Yes. This is the more concerning practice that involves the shifting of financial responsibility to patients rather than the Commercial Insurance Companies. In recent years, Commercial health Insurance companies, including UHC, informed providers that they would be receiving higher payment rates for sessions. However, what ultimately occurred was that the Commercial Health Insurance companies passed those increased costs onto the members, meaning my clients had to bear the burden of higher premiums or out-of-pocket expenses, rather than the commercial health insurance companies paying more themselves. This puts an added financial strain on my clients, many of whom are already facing the complexities of accessing Mental Healthcare.
Soenen: Talk to us about the term “cost-saving.”
Ellison: While Commercial Health Insurance companies claim to advocate for “cost-saving” measures, their tactics often force providers into a corner where we must either compromise the quality of care or face being removed from the network altogether. They sometimes suggest that providers shorten sessions or push for higher billing codes, which doesn't align with patient safety, best practices, or the overall goal of providing quality care.
In some cases, I've been pressured by the Commercial Health Insurance company auditors to read through extensive notes on patients to justify sessions or treatment plans, all of which take away from the valuable time I could be spending with my clients.
Soenen: That is a lot of distress and pressure.
Ellison: The constant shifting of expectations, coupled with the added financial burden on clients, makes it extremely difficult to provide the care that is necessary for their well-being. This, in turn, leads to burnout for providers, who are caught in the middle of trying to serve their patients while navigating a system that doesn’t always align with patient-centered care.
Soenen: In your view, what purpose does Commercial Health Insurance play in Mental Healthcare?
Ellison: In my personal opinion, there is no reason for Commercial Health Insurance industry companies to be for-profit, especially when healthcare is supposed to be a means to access affordable care. While there are advantages in terms of wide network access and preventative care programs that might exist, the system is fundamentally flawed. The way these companies operate often leaves members facing high premiums, deductibles, and out-of-pocket costs that are unsustainable, making care less accessible even to those with insurance.
Soenen: Is this model sustainable?
Ellison: Commercial Health Insurance industry companies like UnitedHealthcare may offer some advantages in the short-term, like a broad network of doctors and hospitals, and coverage for many services, but the broader financial impact on members is undeniable. The premiums, deductibles, and out-of-pocket costs members pay should go directly toward their healthcare needs, but instead, the companies often take those funds and generate enormous profits—sometimes in the billions. For example, despite spending over $14,000 on healthcare this year, even with the best coverage I could find on the MNSure marketplace, I still faced denials and delays on recommended treatments. This system doesn’t prioritize patient care, but rather profits at the expense of those who need the care the most.
Soenen: How does this administrative chaos impact your patients?
Ellison: There are cases where patients cannot receive treatments because the Commercial Health Insurance company won’t cover enough of the cost, making it unaffordable for the member. This kind of denial of necessary care is not only financially harmful to individuals but can lead to long-term health complications, further burdening the system and, ultimately, society.
Soenen: Do you and your colleagues working in Mental Healthcare in Minnesota discuss another approach to, and model of, healthcare? Since the killing of Brian Thompson on December 24, 2024, is there more discussion about what your field of practice desires? What are you hearing?
Ellison: A Single Payer Universal Healthcare system would be transformative and beneficial for both patients and clinicians. With a system where all individuals are covered under one plan, we would eliminate the discrepancies that currently exist within the healthcare system, such as premiums, out-of-pocket costs, and the financial burden that comes with health insurance.
In my experience, when patients or members are on PMAP (Pre-paid Medical Assistance Plans), they are covered by the state, meaning there are no premiums and no out-of-pocket costs for my services. This reduces financial stress for both the client and me as the provider. While the reimbursement per session for these plans may be lower, the consistency in cash flow helps stabilize the practice and provides a predictable financial structure, allowing me to focus on delivering quality care
UnitedHealthcare’s opposition to being excluded from these state plans is not surprising, as these types of programs are a significant way for Commercial Health Insurance companies to generate profit. However, the reality is that these profits are made at the expense of patients’ access to affordable, necessary care.
Minnesota Governor Walz's push to restrict Medicaid contracts to nonprofit entities is a step in the right direction, and I fully support this move. It is a positive shift towards prioritizing patient well-being over corporate profits. That said, the shift towards restricting Commercial Health Insurance companies from participating in these programs may limit members' ability to choose their healthcare coverage, which is a concern.
Balancing accessibility and choice with creating a system that supports patients and providers alike is crucial. Ultimately, the need a system that minimizes barriers to care while fostering sustainability for clinicians is essential. A Single Payer model would be an important step in the right direction, but we must also recognize and address the challenges that come with making such a transition.
“The most frustrating and anger-inducing aspect of the current healthcare system is the clear prioritization of profit over people. The healthcare model, especially within commercial insurance, is designed to work against both patients and providers. For patients, the barriers to receiving necessary care—whether it's due to financial constraints, insurance denials, or overwhelming premiums—are profoundly harmful. As a practitioner, it's heartbreaking to see clients struggle not just with their Mental Health, but also with accessing and affording the treatment they need. It’s demoralizing to witness people being priced out of healthcare, despite having health insurance that’s supposed to protect them.”
-Jessica Ellison, M.A., L.P.C.C.
Soenen: Do you have advice for young persons entering medical school to become Mental Health practitioners now?
Ellison: Entering the field of Mental Health therapy can be incredibly rewarding, but it’s important to understand that, despite being part of the medical field and requiring advanced education, there is not a lot of financial gain in this line of work.
Many individuals pursuing licensure as therapists are often paid very little during their training and are required to complete upwards of 4,000 hours of supervision before they can become fully licensed. Unfortunately, the compensation during this time rarely reflects the level of education or the hours put in. Additionally, with recent potential changes that could restrict supervisors from billing for trainees’ services under their own NPI/Licensure, there will likely be even fewer opportunities for graduates to receive the required supervision they need to become licensed.
Given these circumstances, my advice to anyone entering the Mental Health profession would be to ensure they have adequate financial support to get through the necessary training and supervision hours. If you're committed to this work, be prepared for a journey that may involve financial sacrifices in the short term. However, I would also suggest considering whether this is the right profession in light of the systemic dysfunction in healthcare that is designed to keep professionals underpaid, undervalued, and working within a broken system. Sometimes, it may be worth exploring alternative careers, especially if you're not certain that the long-term rewards outweigh these systemic barriers.
Soenen: What would you like to share Commercial Health Insurance employees, citizens and elected officials who may not comprehend what it is like to be a Mental Healthcare professional in modern day United States?
Ellison: If readers walk away from this with one thing, I want them to understand that the healthcare system is not just broken—it's intentionally designed to make people dependent, fearful, and exhausted. Healthcare providers, despite their dedication, are often left bearing the brunt of a system that puts profits over people, and that has real consequences on both their professional well-being and their personal lives.
Soenen: What gives you hope?
Ellison: Despite the overwhelming challenges in the healthcare system, there is hope. The collective momentum toward systemic change is growing. As more people, including providers, clients, and everyday citizens, begin to speak out and demand better care, we are creating a foundation for meaningful transformation.
The rise of movements like the Minnesota Health Plan, the unionization of medical residents, and the public push for a more compassionate, accessible healthcare system signals a shift in consciousness.
The key is to remain vigilant, to continue advocating for change, and to remind ourselves that we are not powerless. By raising our voices, standing together, and demanding a system that prioritizes health over profit, we can rebuild a healthcare system that truly works for everyone.
The fight isn’t over, and I believe we’re on the verge of a powerful shift.
ADDITIONAL RESOURCES
Investigative Reporting
ProPublica | How UnitedHealth’s Playbook for Limiting Mental Health Coverage Puts Countless Americans’ Treatment at Risk
Coalitions United for Change
Minnesota Trauma Therapist Forum | Newly-formed Support Group
This group is designed to be an open forum for trauma therapists in Minnesota of all degree types and licensures (MFT, Social Work, LP, Ph.D, Psy.D, MA, LPC, LADC, LPCC, Psychiatry, etc.) working in private practices or for organizations.
National Alliance of Mental Health Providers | Dedicated to Transforming the Healthcare Model
NAMHP emerged from a shared sense of frustration and heartbreak felt by Mental Health professionals (LMSWs, LCSWs, LMFTs, LPCs) across the nation—disillusioned by the systemic neglect of Mental Health professionals by legislators, insurance payors, venture capital (VC) and corporate entities. What began as a collective yearning for changing our Mental Healthcare system.
Lorna Breen Heroes Foundation | Dedicated to Preventing Depression vs. Burnout
Lorna Breen is dedicated to suporting the mental health and well-being of all medical professionals in the U.S. by passing legislation and policies that immediately impact governance.
Podcasts
The Nocturnists | The Gilded Age of Medicine with Dhruv Khullar, MD
Physician and New Yorker writer Dhruv Khullar argues that modern medicine is in a Gilded Age—one where groundbreaking innovations mask deep systemic issues, including misaligned incentives, escalating costs, and growing dissatisfaction. From the influence of private equity on healthcare to the flaws of Medicare Advantage and the crucial role of data as the ‘oil’ of the healthcare system, this conversation explores the challenges of contemporary medicine while underscoring the importance of frontline clinicians actively engaging in health policy debates.
Books
In How Do You Feel? Dr. Jessi Gold offers a deeply personal and poignant memoir that explores the hidden tolls of taking care of others. As an assistant professor, practicing psychiatrist, and university wellness leader, Dr. Gold was accustomed to a life of constant busyness, always putting the needs of her patients, colleagues, and loved ones before her own. But when an unthinkable error during a patient session forces her to confront her own mental health, she begins a journey of self-discovery and re-evaluation of the medical system that trained her.
Mental Health Emergency Support
If you, or someone you know, is experiencing a Mental Health Crisis, call 911 immediately or travel to the nearest Emergency Room for medical care.